What Causes Miscarriage? Its stages, Diagnosis & Tests
Miscarriage, also known as spontaneous abortion, refers to the unfortunate loss of a pregnancy before the 20th week. This can occur due to various reasons, and it’s a deeply emotional and challenging experience for individuals and couples. Understanding the causes, symptoms, diagnosis, treatment, and preventive measures surrounding miscarriage is crucial for those who may be affected or supporting someone going through it.
Miscarriage in Different Stages of Pregnancy
First Trimester
In the first trimester is more common and often associated with genetic abnormalities. Understanding the unique challenges of this stage aids in coping and recovery.
Second Trimester
While less frequent, miscarriages can occur in the second trimester. Exploring the reasons behind second-trimester miscarriages provides valuable information for affected individuals.
Third Trimester
In the third trimester, although rare, presents distinct challenges. Recognizing the emotional and physical aspects of late-term miscarriages is essential for those affected.
Most Common Causes Of Miscarriage
1. Medications and Pregnancy Risks
- Certain medications, like Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) and specific antibiotics, can elevate the risk of miscarriage.
- Always consult with healthcare professionals to ensure the safety of any medication during pregnancy.
2. Age as a Significant Factor
- Advanced maternal age is a notable risk factor for miscarriage.
- Individuals planning pregnancies later in life should engage in early family planning discussions and thorough monitoring to address age-related risks promptly.
3. Lifestyle Choices and Pregnancy Outcomes
- Lifestyle choices, including smoking, excessive alcohol consumption, and drug use, are significant contributors to the risk of miscarriage.
- Adopting a healthy lifestyle with regular exercise, a balanced diet, and avoiding harmful substances is vital for supporting a healthy pregnancy.
4. Chromosomal Abnormalities and Genetic Factors
- Chromosomal abnormalities in the developing fetus are among the most common causes of this.
- Early prenatal screenings provide insights into genetic factors, enabling informed decision-making.
5. Infections and Pregnancy Complications
- Infections during pregnancy, such as cytomegalovirus (CMV) and sexually transmitted infections, can significantly increase the likelihood of miscarriage.
- Timely detection, treatment, and adherence to safe practices during pregnancy are essential measures to mitigate the impact of infections on pregnancy.
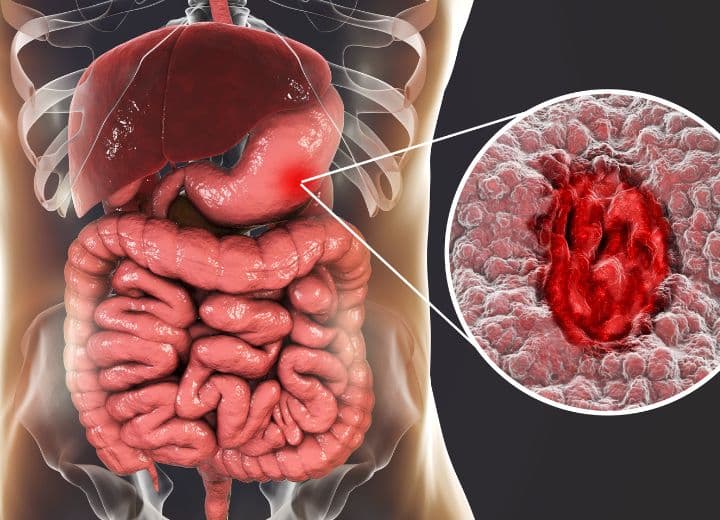
6. Uterine Abnormalities and Structural Issues
- Structural issues with the uterus, such as septate or bicornuate uterus, may pose challenges for implantation and fetal development.
- Surgical interventions may be considered to correct certain uterine abnormalities, enhancing the chances of a successful pregnancy and reducing the risk of miscarriage.
7. Environmental Toxins and Occupational Risks
- Exposure to environmental toxins, especially in occupational settings, can pose risks to pregnancy.
- Minimizing exposure, following safety guidelines, and advocating for a safe work environment are critical measures to protect against environmental factors that may contribute to miscarriage.
8. Stress, Emotional Well-being, and Pregnancy Outcomes
- While the direct link between stress and miscarriage is complex, high levels of stress may contribute to adverse pregnancy outcomes.
- Prioritizing mental health, seeking emotional support, and incorporating stress-reducing activities during pregnancy are essential components of a holistic approach to well-being.
9. Lack of Prenatal Care and Pregnancy Complications
- Inadequate prenatal care may contribute to miscarriage due to the absence of early interventions.
- Regular check-ups, adherence to healthcare recommendations, and active engagement in prenatal care are crucial for a healthy pregnancy and reducing the risk of complications.
10. Rh Factor Incompatibility and Pregnancy Complications
- Rh factor incompatibility between the mother and the fetus can lead to miscarriage.
- Rh testing and appropriate medical interventions, such as Rh immunoglobulin injections, can prevent complications and support a healthy pregnancy.
Diagnosis and Tests
Ultrasound
Medical professionals use ultrasound to visualize the embryo’s development and identify abnormalities. The role of ultrasound in the diagnostic process is pivotal for informed decision-making.
Blood Tests
Blood tests provide valuable information about hormone levels, offering insights into the health of the pregnancy. Interpreting these results aids in understanding the underlying causes of miscarriage.
Tissue Analysis
Analyzing tissue from the miscarried pregnancy can provide conclusive information about genetic factors or other abnormalities. This step is integral for informed family planning decisions.
Treatment Options for Miscarriage: Navigating the Path to Recovery
Experiencing a miscarriage is a challenging and emotional journey, and understanding the available treatment options is crucial for individuals seeking support and healing. Here, we explore the various approaches to managing and recovering from a miscarriage.
1. Expectant Management
Expectant management, often known as “watchful waiting,” is a conservative approach where healthcare providers monitor the natural progression of the miscarriage without immediate medical intervention. This option is considered when there are no signs of infection or excessive bleeding. It allows the body to expel pregnancy tissues naturally over time.
2. Medications to Facilitate Miscarriage Completion
In some cases, healthcare providers may prescribe medications to help facilitate the completion of this.
Common medications include:
– Misoprostol:
This medication helps the uterus expel pregnancy tissues and is often used in conjunction with expectant management.
– Mifepristone (RU-486):
Administered under medical supervision, mifepristone is another option to induce the completion of a miscarriage.
The choice of medication depends on individual health factors and the specific circumstances surrounding the miscarriage.
3. Surgical Procedures
When necessary, surgical procedures may be recommended to remove remaining pregnancy tissues and prevent potential complications.
Two common procedures are:
– Dilation and Curettage (D&C):
In this procedure, the cervix is dilated, and the uterus is scraped to remove any remaining tissues.
– Dilation and Evacuation (D&E):
Similar to D&C but performed later in pregnancy, D&E involves the use of suction and medical instruments to remove pregnancy tissues.
Surgical procedures are typically considered when other methods are not effective or in cases of incomplete miscarriage.
4. Emotional Support and Counseling
Coping with the emotional impact of a miscarriage is a crucial aspect of treatment. Healthcare providers may recommend seeking emotional support from counsellors, therapists, or support groups. Counselling can provide a safe space for individuals and couples to express their feelings, navigate grief, and develop coping strategies.
5. Follow-up Care and Monitoring
After the completion, follow-up care is essential to monitor physical and emotional well-being. Regular check-ups with healthcare providers allow for assessing recovery progress and identifying any potential complications.
6. Fertility Counseling
For individuals who desire to conceive again after this, fertility counselling may be recommended. Fertility specialists can provide insights into potential underlying causes of the this, offer guidance on family planning, and address concerns related to future pregnancies.
7. Addressing Underlying Health Conditions
In cases where underlying health conditions contribute to recurrent miscarriages, healthcare providers may initiate investigations to identify and address these issues. This may involve hormonal evaluations, genetic testing, or assessments of uterine health.
8. Grief Support and Coping Strategies
Grieving is a natural and individual process, and seeking grief support is essential. Healthcare providers may recommend resources such as grief support groups, online forums, or specialized counselling services to assist individuals and couples in navigating the emotional aftermath of a miscarriage.
Also, Read this: Vaginal Cysts:Causes, Symptoms,Treatments
Conclusion
Navigating the treatment options that involves a personalized approach that considers both the physical and emotional aspects of recovery. Seeking support from healthcare professionals, emotional counselling, and follow-up care contribute to a comprehensive and empathetic journey toward healing.
Frequently Asked Questions(FAQ)
How can age impact the risk of miscarriage?
Advanced maternal age is associated with an increased risk of miscarriage. Early family planning discussions and monitoring are essential for older individuals.
What lifestyle choices contribute to miscarriage risks?
Lifestyle choices, including smoking, excessive alcohol consumption, and drug use, are significant contributors to the risk of miscarriage. Adopting a healthy lifestyle is vital for a healthy pregnancy.
How can infections affect pregnancy outcomes?
Infections during pregnancy, such as CMV and sexually transmitted infections, can significantly increase the likelihood of this condition. Timely detection, treatment, and safe practices are crucial.
Is Rh factor incompatibility common in pregnancies?
Rh factor incompatibility between the mother and the fetus can lead to this condition. Rh testing and appropriate medical interventions can prevent complications and support a healthy pregnancy.
Can specific medications increase the risk of miscarriage?
Certain medications, such as NSAIDs and some antibiotics, may pose a risk. Always consult with a healthcare professional before taking any medication during pregnancy