What Is Peptic Ulcer? Causes, Symptoms, Treatment.
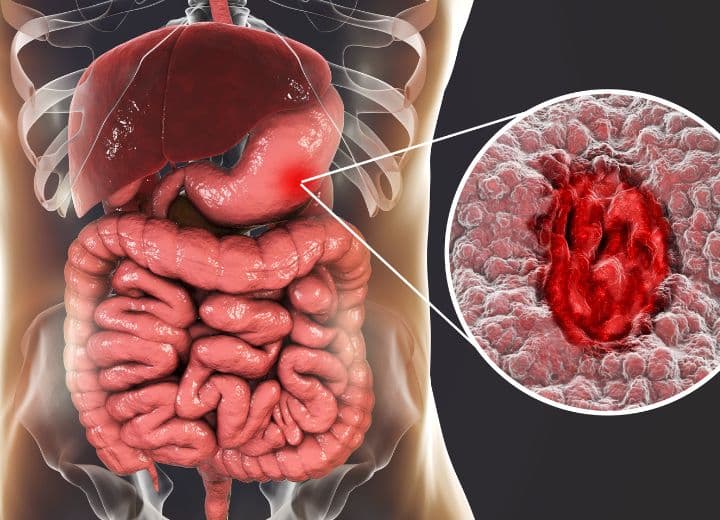
Peptic ulcer refers to an open sore or lesion that forms on the stomach’s inner lining or the small intestine’s inner upper part. These ulcers develop when the protective layer of mucus that lines the stomach and duodenum (the initial part of the small intestine) is compromised, allowing stomach acid to erode the underlying tissue.
Types of Stomach ulcer
There are different types of ulcers, each with its own characteristics and locations. The two main types of ulcers are gastric ulcers and duodenal ulcers.
Gastric Ulcers:
Definition: Gastric ulcers occur in the stomach lining.
Location: These ulcers develop on the inside of the stomach.
Symptoms: Patients with gastric ulcers may experience pain shortly after eating.
Duodenal Ulcers:
Definition: Duodenal ulcers form in the upper part of the small intestine, known as the duodenum.
Location: These ulcers are located in the first section of the small intestine.
Symptoms: Pain from duodenal ulcers is often felt a few hours after eating.
“Understanding the type of ulcer is essential for effective diagnosis and treatment. Gastric and duodenal ulcers may have similar symptoms, but the location and timing of pain can provide valuable clues for healthcare professionals in determining the type of ulcer a patient may have.”
Causes Of peptic ulcer:
The causes of peptic ulcers are multifaceted, involving various factors that contribute to the development of these painful sores on the inner lining of the stomach or the upper part of the small intestine. Here are the primary causes:
Helicobacter pylori Infection:
This bacterium, known as H. pylori, is the most common cause of ulcers. It infects the stomach lining, weakening the protective mucous layer and making the stomach more susceptible to the damaging effects of gastric acids.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs):
Regular use of NSAIDs, such as aspirin, ibuprofen, and naproxen, can lead to the development of peptic ulcers. These medications can irritate the stomach lining, reduce the production of mucus, and increase stomach acid secretion.
Stress and Lifestyle Factors:
High stress levels and certain lifestyle choices, including smoking and excessive alcohol consumption, are associated with an increased risk of ulcers. Stress may exacerbate existing ulcers and delay the healing process.
“Understanding these causes is crucial for both prevention and treatment. Addressing the underlying factors can help manage ulcers effectively and reduce the risk of recurrence. If you suspect you have a peptic ulcer, seeking medical advice for proper diagnosis and tailored treatment is essential.”

Symptoms Of peptic ulcer:
Peptic ulcers can manifest with a variety of symptoms, ranging from mild discomfort to more severe pain. Here are some common symptoms associated with peptic ulcers:
Burning Sensation:
Individuals with peptic ulcers often experience a burning or gnawing sensation in the upper abdomen. This discomfort is typically felt between meals and can be temporarily relieved by eating or taking antacids.
Abdominal Pain:
Persistent abdominal pain is a hallmark symptom of peptic ulcers. The pain is usually located in the upper abdomen and may vary in intensity. It can come and go or remain constant.
Nausea and Vomiting:
Peptic ulcers may cause feelings of nausea, and in some cases, individuals may experience vomiting. These symptoms are often more pronounced on an empty stomach.
Changes in Appetite:
Some people with peptic ulcers may notice changes in appetite, ranging from a decrease in interest in food to feelings of early satiety.
Unexplained Weight Loss:
Long-term ulcers can lead to unintentional weight loss due to factors such as reduced appetite and difficulty in maintaining a normal diet.
Bloating and Burping:
Excessive gas, bloating, and burping may occur as a result of the irritation caused by the ulcer on the stomach or duodenal lining.
Dark or Bloody Stools:
In more severe cases, peptic ulcers can lead to gastrointestinal bleeding. This may manifest as dark, tarry stools or the presence of blood in vomit.
Chest Pain:
Some individuals with ulcers may experience chest pain, which can be mistaken for heart-related issues. This pain may radiate to the back.
“It’s important to note that symptoms can vary from person to person, and some individuals may not experience any noticeable symptoms. If you suspect you have peptic ulcers or are experiencing persistent abdominal pain, it’s advisable to seek medical attention for a proper diagnosis and appropriate treatment.”
Diagnosis of ulcer:
Diagnosing involves a combination of medical history assessment, physical examination, and specific diagnostic tests. Here are common methods used in the diagnosis of peptic ulcers:
Medical History:
The healthcare provider will begin by taking a detailed medical history, including a discussion of your symptoms, their duration, and any factors that may exacerbate or alleviate the pain. Information about medications, lifestyle, and diet is also important.
Physical Examination:
A physical examination may be conducted to assess signs of abdominal tenderness, bloating, or any unusual sounds in the abdomen. The healthcare provider may also check for other potential causes of abdominal pain.
Endoscopy:
Endoscopy is a commonly used procedure for diagnosing peptic ulcers. A thin, flexible tube with a camera (endoscope) is inserted through the mouth and into the esophagus, stomach, and duodenum. This allows the doctor to directly visualize any ulcers, take tissue samples for biopsy, and assess the severity of the condition.
Barium X-ray:
A barium X-ray, also known as an upper gastrointestinal (GI) series, involves drinking a barium solution before X-rays are taken. The barium outlines the stomach and duodenum, making ulcers visible on X-ray images.
Blood Tests:
Blood tests may be conducted to check for the presence of Helicobacter pylori antibodies or to identify signs of anemia or infection. Elevated levels of certain enzymes may also indicate inflammation.
Stool Tests:
Stool tests may be performed to detect the presence of blood, which could indicate gastrointestinal bleeding associated with peptic ulcers.
Pylori Tests:
Specific tests may be conducted to detect the presence of Helicobacter pylori bacteria. This can include breath tests, blood tests, or stool tests.
CT Scan or MRI:
In certain cases, imaging studies like computed tomography (CT) scans or magnetic resonance imaging (MRI) may be used to identify complications or assess the extent of the ulcer.
The combination of these diagnostic methods helps healthcare professionals accurately diagnose peptic ulcers, determine their cause, and formulate an appropriate treatment plan. If you suspect you have peptic ulcers or are experiencing persistent abdominal pain, it is essential to consult with a healthcare provider for proper evaluation and diagnosis.
Treatment OF Peptic Ulcer:
The treatment of peptic ulcers typically involves a combination of medications, lifestyle changes, and, in some cases, addressing the underlying causes. Here’s an overview of the common approaches to treating peptic ulcers, along with a list of medications often used:
Proton Pump Inhibitors (PPIs):
PPIs are a class of drugs that reduce stomach acid production, promoting healing of the ulcer and preventing its recurrence. Examples include:
- Omeprazole (Prilosec)
- Esomeprazole (Nexium)
- Lansoprazole (Prevacid)
Histamine-2 (H2) Blockers:
H2 blockers reduce the amount of acid the stomach produces. They can be used in place of PPI or used in combination with PPI to enhance efficacy. Examples include:
- Ranitidine (Zantac)
- Famotidine (Pepcid)
- Cimetidine (Tagamet)
Antibiotics:
If the peptic ulcer is caused by Helicobacter pylori infection, a course of antibiotics is prescribed to eradicate the bacteria. Commonly used antibiotics include:
- Amoxicillin
- Clarithromycin
- Metronidazole
- Tetracycline
Antacids:
Antacids provide quick relief by neutralizing stomach acid. They are often used for symptomatic relief and can be taken as needed. Examples include:
- Aluminum hydroxide
- Magnesium hydroxide
- Calcium carbonate
Cytoprotective Agents:
These medications help protect the lining of the stomach and duodenum Such as Sucralfate
Mucosal Protectants:
Medications like misoprostol may be prescribed to enhance the protective mucus lining of the stomach and reduce the risk of ulcers caused by NSAIDs.
Lifestyle Changes:
Making certain lifestyle modifications can aid in the treatment of peptic ulcers.
These may include:
- Avoiding spicy and acidic foods
- Limiting alcohol consumption
- Quitting smoking
- Managing stress through relaxation techniques
Conclusion:
In conclusion, peptic ulcers demand attention and a multi-faceted approach to treatment. From accurate diagnosis through endoscopy and tests to targeted medications like PPIs and antibiotics, managing these ulcers requires both medical intervention and lifestyle adjustments. Combining dietary changes, stress reduction, and regular check-ups creates a comprehensive strategy for effective ulcer management. With proper care and awareness, individuals can lead fulfilling lives despite the challenges posed by peptic ulcers.
Also Read: What is Sleep Paralysis?
FAQs (Frequently Asked Questions) :
Q: Can stress alone cause peptic ulcers?
A: While stress is not the sole cause, it can contribute to their development. Managing stress through relaxation techniques is important for overall digestive health.
Q: Are all peptic ulcers caused by Helicobacter pylori infection?
A: No, not all peptic ulcers are caused by H. pylori. Other factors, such as NSAID use and lifestyle choices, can also contribute. Identification of the underlying cause is crucial for effective treatment.
Q: Can peptic ulcers be cured completely?
A: Yes, peptic ulcers can be cured with appropriate treatment. Medications like antibiotics, proton pump inhibitors, and lifestyle changes play a key role in promoting healing and preventing recurrence.
Q: Is there a specific diet for managing peptic ulcers?
A: While there’s no one-size-fits-all diet, individuals with peptic ulcers are often advised to avoid spicy and acidic foods. A balanced diet rich in fruits, vegetables, and whole grains is generally recommended.
Q: Can I take over-the-counter antacids for peptic ulcers?
A: Over-the-counter antacids can provide temporary relief from symptoms, but they are not a long-term solution. Consult with a healthcare professional to determine the most appropriate medications and treatments for your specific condition.